Thursday, December 26, 2013
Merry Christmas or Whatever You Want to Call It
Sunday, December 8, 2013
Controlled substances
There are a lot of important issues facing our hospital right now. We are in an old poorly constructed building where elevators freeze and pipes burst regularly. Our emergency is plugged up with patients waiting to be admitted because there are no beds available. Our operating room has been told it has to cut $800,000 from its budget (without cancelling any cases apparently). All good reasons for a large meeting of the minds. None of these were what the meeting was about however.
The purpose of the meeting was to discuss the hospital's Controlled Substances Policy.
Anaesthesiologists are alone among physicians in directly administering narcotics to patients as opposed to giving an order and having a nurse administer narcotic. We give short acting narcotics like fentanyl and remifentanyl for induction and maintenance of anaesthesia and we give longer acting agents like morphine or hydromorphone for analgesia. We give drugs by bolus, we give them by infusion, intravenously, epidurally or intraspinally. We also use controlled drugs like ketamine. Some other drugs we use are not (yet) controlled but are prone to abuse like propofol and midazolam.
When a nurse wants to give a controlled drug, she has to get the drug from a locked cabinet (usually after tracking down the nurse who has the keys), count what is in the locked cabinet usually with another nurse, write the drug in the narcotic book, give the drug to the patient and if the full dose isn't given, the wastage must be verified again witnessed by another nurse. This is while the patient who was told not to ask for analgesia until it was REALLY necessary is writhing in pain, pushing the call button.
At our hospital we do things a little differently in the OR. At the beginning of the day, based on what I think I will need, I log into our Pyxis machine and sign out whatever I think I will need for the day. I generally leave them on top of my anaesthetic cart. I do write down what I give to the patient on the anaesthetic record but when I want to discard any drug, say for example I only give 5 mg or a 10 mg morphine amp, I just throw it in the sharps container without any witness. Quite often I may split an ampoule between 2 or more patients. Remifentanyl for example I dilute to 100 mcg per cc and use 50-100 mcg on induction using of course a clean syringe for each patient. I like remifentanyl infusions, to save time I often mix up a whole bunch at one time and then divide it amongst patients. I could just use a separate 1 mg remifentanyl ampoule for the 100 mcg dose on each patient at $40 per ampoule but somewhere in my pedigree there was a Scotsman who reminds me that this is wasteful. In addition the drug shortages we have recently experienced makes it all the more attractive not to waste drugs.
At various times in various hospitals I have had to fill out narcotic sheets where we write the patient's name (or use a sticker) and write down what we gave them. Most of us gave this up when we found out that nobody actually read these sheets. Besides we already document the dose on our anaesthetic record.
At the end of the day I could sign the drugs I didn't use back into the Pyxis but why bother? I just lock them in my locker and use them the next day. This is by the way legal in Canada for physicians.
Propofol and midazolam are supplied on my anesthetic cart at the beginning of each day and restocked as necessary. Because we spotted somebody (not an anesthesiologist) flitting around the ORs one evening probably sniffing gas, we now secure our anaesthetic carts with a plastic tie, just in case somebody is helping themselves to the odd vial of propofol or midazolam. (We decided not to lock them because we know the key will inevitably be lost.)
At some hospitals a narcotic kit is dispensed containing a sampling of various narcotics that can be used during the day. This entire kit can be signed back in so that pharmacy can keep track of what has been used. Stocking these kits is very labour intensive for pharmacy who hate them which is why we don't use them at our hospital.
Apparently a couple of times a week, there is a discrepancy between the amount of drugs dispensed, the amount returned and what is left in the Pyxis, which is a headache for nursing and pharmacy but up until now not for me. I have no idea of what type of skulduggery is necessary to resolve these discrepancies and really don't intend to try to find out.
All this is causing dyspepsia for the Stasi lady from our quality department who is behind these meetings.
The result of the meeting was that we all lost an hour of our lives and came no closer to the solution. Most people gently pointed out that doing anything like what the Stasi-lady wanted was clearly impractical and most likely impossible. Pharmacy pointed out that they would need more resources if the letter of the law was to be followed. I pointed out the impracticality and futility of charting wastage of narcotics in a busy OR. We will meet again sometime in the future when 20 or so people can find a mutually acceptable spot in their timetable. I expect to be able to string this out until I retire.
Aside from it being the law, what is the big fuss?
Drug diversion certainly is a problem although probably less of a problem than some people would make it out to be. Drug use is a problem in a small minority of anaesthesiologists although we are apparently more likely to abuse injectable narcotics than our colleagues who don't have the same access. (I interview prospective residents and I have not yet met somebody who said that he wanted to go into anaesthesia because of the easy access to narcotics.) Abuse of injectable narcotics has three issues. There is first the illegality of it, second the effect on the health of the abuser and most importantly the effect on patients of being cared for by an impaired anaesthesiologist.
When anesthesiologists are caught, as has been pointed out over and over again, it is not because of tight narcotic controls and documentation; it is because of behavioural changes. Narcotic addiction is a horrible problem but alcohol abuse and addiction is probably a worse problem among physicians. The biggest cause of impairment in physicians is fatigue, something I have never heard administration expressing any concerns about.
The bottom line is, you do have have to trust people a little but at the time realize that they can and will screw up and be vigilant against this.
Lost among this discussion is the patient. We give narcotics for a reason. We give morphine for pain because despite all its downsides we haven't yet found a better way to deal with pain. We use the fentanyl family because they blunt the response to intubation and are cardio-stable. Just how important these properties are is questionable but most of us like them. Remifentanyl with its short half life is a great drug for induction and maintenance of anaesthesia. Any time you make narcotics harder to use, a significant proportion of docs and nurses will just say, "to hell with it" and not use them which means that the patient will suffer.
As I said to somebody as we left the meeting, "the hospital has way worse problems than this.""
Friday, November 29, 2013
Commercials on "free" Wifi WTF?
I went to Starbucks for a coffee and pastry yesterday. Unlike most coffee shops which have "free" newspapers lying around, Starbucks doesn't, which left me to check the internet on my I phone while I drank my Grande dark roast. I am not one of the those people I see a lot lately at Starbucks, usually sitting by themselves at a four person table with their laptop, obviously there for the long haul, but I do like to use their free internet while drinking my overpriced coffee and second rate pastry.
Not so free any more. I found that their free internet is now sponsored by Travel Alberta and before I could access my internet I had to watch a 30 second commercial on my phone.
Aside from having to watch the commercial (which I have already seen on TV), why would my government spent $$$ preparing this video and then paying Starbucks $$$ to force me to watch it, all with the goal of getting me to visit Alberta, when I already live here?
Unfortunately I suspect we are going to be getting a lot more commercials with our free internet.
Thursday, November 21, 2013
If You Were Wondering Where I was on November 22, 1963.
I came home from school for lunch. Our school was only a couple of blocks away from our house and so I walked home by myself at lunch and after school. My mother who, like almost every mother on the block, didn't work always made lunch for my brothers and me. I was in Grade I. When I got home my mother told me that President Kennedy had been killed. Although I was six and Canadian I sort of knew who he was. We ate lunch and I went back to school.
Our teacher told us again that President Kennedy had been killed. At about 2 o clock the principal came on the PA and told us that under the circumstances we should all go home early. I don't remember being that happy about getting out early.
Later I remember watching the funeral.
Since then there have been many what ifs and conspiracy theories.
If you want a good what if, National Lampoon devoted a whole issue to it in 1977.
I suspect that JFK hadn't been assassinated, he probably would have won a second term during which time any honeymoon he may have had with the American voter might have ended and unfortunately we would had probably still ended up with Nixon, Reagan and the Bushes in the future.
Likewise I have read or heard all the conspiracy theories. It seems I can't turn on History or Discovery channel lately without seeing another one. Maybe I am fatigued by everything but I have come to believe that you had a serious nutcase Oswald, who just got off a lucky shot and maybe Jack Ruby was just really pissed off that the President died. Maybe that is what they want me to believe.
Shouldn't have happened.
Monday, November 11, 2013
K.I.S.S.
 KISS as we all know stands for Keep It Simple Stupid (or Keep It Simple Sweetheart). I first heard this in medical school from a surgeon who started his lecture by writing this on the blackboard.
KISS as we all know stands for Keep It Simple Stupid (or Keep It Simple Sweetheart). I first heard this in medical school from a surgeon who started his lecture by writing this on the blackboard.Surgery is easy.
I am not saying anybody can do it but if you get into medical school, graduate, do a surgery residency and do enough of the basic procedures you should be able to function. Most procedures have already been done before by somebody else, anatomy is relatively constant and tools have been designed to make things easier. Not only that, you work with scrub nurses who can anticipate what you are going to do and anaesthesiologists who look after your patient for you and provide muscle relaxation. Surgery should be really boring which is why historically surgeons have tried to make it more difficult by working when they are tired and doing unnecessary surgeries.
And then the laparoscope was born.
Laparoscopy was originally used by gynaecologists mostly for tubal ligations but also for diagnostic laparoscopies. The anatomy of the uterus, tubes and ovaries is pretty simple and even in the old days, looking thru an eyepiece they could safely and effectively do their work.
It took general surgeons a little bit longer to get on the laparoscopic bandwagon with the laparoscopic cholecystectomy. Those of us who worked in the era of the introduction of the laparoscopic cholecystectomy remember this as a dark time in the anaesthesiology world. Surgeons would go away for a weekend course where they operated on a pig or cadaver and would return raring to get onto the future of surgery. They would show up in the OR usually with a rep from the company who sold the expensive equipment and a three hour ordeal of fiddling around would begin innevitably followed by the open cholecystectomy. This would be repeated multiple times over the next year or so and usually multiple general surgeons were learning to do these so you can imagine the chaos in the OR, especially when they realized that it was affecting their elective time and started doing them afterhours. There were also the common duct injuries, about 20% in the early stages requiring a long tedious repair by another surgeon.
Today laparoscopic cholie is the standard, most surgeons can run one off in about an hour as a day case and nobody would think of subjecting a patient to a subcostal incision. There are a few problems with the laparoscopic cholie however. Firstly the cholecystectomy rate has gone up since the introduction of the lap cholie. There are two reasons for this. Firstly patients faced with the prospect of a painful subcostal incision may decide to just live with the occasional bout of gut grief. A significant number of surgeries are for assymptomatic gall stones. Secondly instead of a procedure which keeps a patient in hospital for several days, surgeons now have a procedure which is either a day surgery or at the worst an overnight stay. And of course the old open cholies which kept patients in hospital beds for days, deterred surgeons from doing them as "emergencies" lest their elective cases be affected by "emergency" cases occupying their beds. Not a problem with the laparoscopic cholie. It is now a rare evening or weekend on call that I don't do at least one of these. Therefore we are doing more cholies and more of them after hours. And don't forget that even in the most skilled of hands this is a procedure associated with the occasional complication. What about post-op pain? It seems that laparoscopic cholie is still pretty painful maybe not as much as open but instead of getting morphine in hospital lap cholie patients go home with Tylenol with Codeine.
Having mastered albeit slowly the cholecystectomy surgeons moved on to other easy procedures that they could now make more difficult.
We have laparoscopic appendectomy. These can now be done in about an hour by a competent general surgeon longer if they let the second year resident do it. Are they any better than the open appy. Remember most good general surgeons could do these thru a keyhole incision which is about as long as the total length of the four little incisions necessary to do it laparoscopically. And the length of stay and complication rate is the same as open which costs only one third as much. At least laparoscopic patients can wear a bikini afterwards if you forget the ugly scar in the umbilicus. Appendicitis as I tell surgeons is a medical disease now.
Laparoscopic hernia repair is now fashionable as well. The problem with this type of surgery is that many of the patients who get hernia repairs are older patients with coexisting disease. Patients you would like to do under spinal or local (or tell them to wear a truss for the rest of their lives). Instead you end up fighting inflation pressures in the COPDer you are doing under general instead of spinal. Plus you have to use mesh. Being in practice many years, I have absorbed many hours of surgical teaching and remember the admonitions of staff surgeons in the 80s and 90s to avoid using mesh whenever possible due to risk of infection. Either way hernia repair is a day procedure whether done locally or laparoscopically. Laparoscopic hernia repair costs several times as much.
Don't get me started on laparoscopic bowel resection. The feeling is only now
returning to my bum after the epic-ally long procedure I did last week. The purpose of laparoscopic surgery is surely to spare the patient an abdominal incision. Except that the bowel has to come out somewhere which requires a 10 cm long incision to remove the bowel. So you get a surgery which takes twice as much time, done semi-blind and you still end up with a fairly substantial incision. Incisional pain can be handled of course with an epidural which our surgeons don't like us doing when they get out the laparoscope.
Urologists have gotten into the act with laparoscopic nephrectomies and adrenalectomies. (Technically as these are retro-peritoneal structures these are not laparoscopies). We thankfully don't do them at our hospital so my only knowledge is from hearing of the horrendous complications like the urologist who got into the inferior cava doing a laparoscopic adrenalectomy. Urologists have also gotten into robotic surgery with great gusto despite data suggesting that the complication rate is the same as the open procedure which is cheaper and takes less time. Plus in order to do the robotic prostatectomy urologists want the patient in extreme head down position which has lead to significant post-op confusion and who knows what long term CNS changes.
Gynaecologists who of course pioneered laparoscopic surgeon have moved on from tubals and lysis of adhesions. I have recently done two laparoscopies for bleeding ectopics who came to the OR shocky. My first response when they got out the laparoscopic equipment was, "surely you can't be serious?" but I am such a wimp. Bleeding, especially arterial bleeding, looks 10X as bad blown up on the TV screen. We also have the laparoscopic assisted hysterectomy which is really just a glorified vaginal hysterectomy. Vaginal hysterectomy which was historically done blind had an incredibly low complication rate. The last laparoscopic assisted hyst I did came back a few days later because her bowel had been perforated. And this is just to avoid a Pfanensteele? incision. I am waiting for my first laparoscopic Caesarian Section and don't think somebody isn't thinking about this.
I could rant on about all the other "minimal access" surgeries being done in other surgical specialties.
I am not against progress, if I had my gall bladder out, I would want it out laparoscopically. Not so much my appendix and definitely not a hernia repair (I would have this under local). The thing is, doing something just because it is neat, doesn't justify the procedure and sometimes there is a reason why things have been done the way they were done for many years.
Saturday, November 2, 2013
If I collapse at work, here is a list of doctors that I don't want working on me.
At the recent ASA meeting, I attended 2 separate ethics sessions which dealt with the same question. If you know the surgeon is incompetent and the patient asks you, do you tell them? The ethical answer is yes, however you could see how this would play out in the workplace should you actually do this.
A while ago I got a phone call from an exasperated colleague complaining about one of our surgeons. This surgeon more or less restricted his practice to certain area but when on call takes on all comers. My colleague pointed out that this surgeon had taken way longer than other surgeons to do a case with the result that that OR was now backed up with emergencies. I had gotten the same impression so a day or so later I ran into the Chief of Surgery in the lounge and raised the question. I obviously wasn't the first person to do so. "His infection rate is the same as everybody else and his length of stay is the same too," spat out the Chief. I later talked to the Chief of Staff, also a surgeon, and got the same answer. Hmmm I thought if both of them know this surgeon's average length of stay and infection rate, maybe they had to look into it for some reason.
We had a now departed cardiac surgeon at the Centre of Excellence who was to say the least not very good. Bad to the extent that several cardiac anaesthesiologists actually gave up doing cardiac anaesthesia rather than work with him ever again. That's right cardiac anaesthesiologists actually gave up lucrative work because they didn't want to work with a surgeon. (Some of them later rejoined on the condition that they not have to work with this surgeon). One female anaesthesiologist said she felt like a murdress every time she worked with this surgeon. One day a bunch of them were talking in our lounge about how bad this surgeon was, when I interjected, "Do you think you may be liable for working with him when you think he is incompetent?". "That's an interesting question," replied the department chairman who had made a rare appearance to sit with the little people. This is unlike this group of anaesthesiologists at another centre who had the cojones to refuse to work with a clearly incompetent cardiac surgeon and saved countless lives.
The surgeon at the CofE continued to work on for a couple more years after this and is now working somewhere in the US interestingly enough as an anaesthesiologist, as I found out on Google, which is surprising given his poor opinion of anaesthesiologists when he worked in Canada.
There are two components to surgery. One is technical skill and one is judgement. A surgeon may have perfect technical skills but very poor judgement and inappropriate surgery well performed can be as bad as appropriate surgery badly performed.
Incompetent surgeons come can be divided into groups.
Some surgeons are just plain incompetent.
Other surgeons learn early on that they cannot handle difficult cases and restrict their practice to a small menu of cases that they know they can do. That is assuming there are any cases that they are able to do. This works out especially if they work with someone who can occasionally bail them out.
The most dangerous surgeon is the surgeon who doesn't know he is incompetent. Some of these are idiots who just blissfully ignore their bad results. Quite a few of them a sociopaths who don't care about their bad results. I suspect a large number of these surgeons actually know they are incompetent but have invested too much time and training and are working away waiting to get found out. There is a subgroup who do some types of surgery quite competently but will attempt more difficult surgery with terrible results. Quite often these individuals claim to be subspecialists in the very area they lack competence in.
A lot of us will actually tolerate an incompetent surgeon if he is pleasant to work with, works reasonably fast, doesn't do a lot of cases after hours and his cases don't come back to the OR too often. The incompetent surgeon who is a complete asshole may get caught out sooner or conversely concerns about his work may be downplayed as "you are just complaining about him because you don't like him." Or of course if he is a complete sociopath people including anaesthesiologists may be afraid to complain.
OKAY SO WHAT ABOUT INCOMPETENT ANAESTHESIOLOGISTS.
Yes they exist. Some are globally incompetent, some may just have trouble with certain aspects of care like epidurals for example. When I first started out there were still a large number of anaesthesiologists with little or no formal training who had been grand-fathered in and were still working even in large centres.
Surgeons like most bad anaesthesiologists because they rarely do regional blocks, art lines or central lines, they cut corners and never cancel cases except for the bad anaesthesiologist who has enough insight into his skills and only will do ASA 1 cases. Further bad anaesthesiologists usually don't mind working after hours and will stay late. Some surgeons know that the anaesthesiologist isn't really that good and just try to avoid him for their sicker patients. Bad anaesthesiologists are either really nice guys so the nurses and the surgeons put up with the badness or they are real assholes and everybody is afraid to confront them.
Years ago there was an older anaesthesiologist whose skills had slipped which culminated in a surgeon finally refusing to work with him while on call. This was a shock to everybody. This individual did continue to work on for a few more years but wasn't allowed to take call, an imperfect compromise. At our hospital we had to get rid of two anaesthesiologists about 5 years ago. They had been there for years after training in another country. It had been suspected for years that they less than competent but the surgeons loved them because they worked fast, never canceled cases for medical reasons and loved to work after hours. Our department chief was forced to do a prolonged chart review of all their cases before he found enough evidence to hang them which he did and they retired. All in all less than pleasant.
Friday, October 4, 2013
Good thing that Hypocratic Oath.
There is a Doonsbury cartoon about 30 years ago, based on Henry Kissinger's CABG surgery. In the cartoon the surgeon is talking with Kissinger a day or so post-op. He notes that during the surgery he was holding the heart of somebody who had condemned thousands to death. He said, "Then I thought of my Hypocratic Oath and sewed you up". Kissinger replies, "Good oath that".
A couple of months ago while working I went out to see a patient for a procedure. His name seemed familiar so I thought that he might have been a patient I had seen before or even somebody I might have have met socially. I asked him that and he said he didn't remember meeting me.
It was only after I put him to sleep that I realized the man who had placed his life in my hands was the insurance assessor I wrote about here.
I told the staff in the room about him and what he had put me through but at the end of the case I took him to the recovery room and went on with my business (I even gave him something for nausea) and presumably a day or so later he went on with his business and I hope to god we never meet one another again.
Open Letter to Your Friendly Emergency Room Doctor
Emergency room doctors certainly write a lot of blogs and rants, and they do have the most interesting stories which is is probably why they have TV shows about the ER and not about anaesthesia.
I have seen variations on this rant before either from ER doctors and nurses. I thought it was pretty fun but then I thought about the patients I see in the pain clinic and how I used to treat chronic pain patients when I worked in the ER and how chronic pain patients get treated now. Therefore.
OPEN LETTER TO YOUR FRIENDLY EMERGENCY ROOM DOCTOR.
I worked a lot of emergency shifts before I became an anaesthesiologist, both as a family doctor, and as an "emergency room physician", so I actually have some empathy for what you face and I agree with about 90% of what you say. However as a chronic pain doctor who follow chronic pain patients and writes prescriptions for oral opioids, I have to make the following points.
There are a lot of slime balls out there who like to try to fool unsuspecting doctors but there are also a lot of legitimate patients who suffer from either acute or chronic pain. The problem is the tendency to lump all these patients into a single group.
When my patients ask about going to the emergency room, I tell them that the emergency room is for people with fractures and heart attacks and that their chronic back pain is not an emergency. I try to give them some treatments and get them some skills to avoid visiting the emergency. And for the most part the patients I follow don't visit the emergency. I know this know because all emergency records are posted on our province's EMR and I check this. And many of my patients who have been to the emergency describe it as the worst experience of their lives, something they would do anything to avoid. Having said this, patients with chronic pain who take opioids do break bones, or get appendicitis. This is usually a horrible experience for them because most ER docs don't give enough analgesia to normal patients let alone narcotic tolerant patients.
Many of the problems I see in the pain clinic are the result of bad treatment in the ER. Take the episodic migraine patient who has been transformed into a chronic daily headache patient by all the injections of various narcotics, sedatives and anti-inflammatories that ER docs like to give because we all know every ER doc is an expert on treating headaches. Did it occur to you that maybe some of these patients weren't just drug seeking and were actually looking for some type of long term solution. All yeah, ER docs don't do follow up; that's what you like about ER.
Given all the bad side effects and long term consequences of NSAIDs (which all ER docs know about because they were in the top 25% of their class), is it surprising that patients maybe don't want to take them? Especially when they may have been popping OTC NSAIDs all day before they decided to go into the ER. And what is the fascination among ER docs with ketorolac (Toradol)? While it was marketed aggressively by the company as an analgesic, it is an NSAID just like all the other NSAIDs except that it can be injected. Every time I see somebody with marginal renal function who has received multiple doses of ketorolac in the ER, I shudder. None of the patients I see in the pain clinic are allergic to Tylenol. In fact one of the hardest jobs I have in the pain clinic is convincing patients not to take so much Tylenol and acetaminophen containing compounds. In Canada you can buy acetaminophen 325 mg with 8 mg of codeine and that is pretty popular. (Confession: I even get some for myself if I have a really bad cold/flu). This is posted on the patient's EMR now as well and it is interesting just how much of this some patients buy.
And why wouldn't a patient ask for a drug that he know has worked in the past? When I had a dental abscess, tylenol with codeine didn't work percocet did. Guess what I'm asking for next time?
And patients do lose prescriptions and have them stolen. If you lose your BP pills, you just call the pharmacy and they will give you another batch. Because of regulations, pharmacies can't or won't refill your opioid prescription without calling your doctor. Quite a few of my chronic pain patients lose their prescription or have it stolen. This only ever happens once. Likewise occasionally when patients run our of medication, they find that their family doctor is on holidays, has retired, or the office tells them that the next available appointment is in 2 weeks. Sure patients should plan to get their prescriptions filled when their doctor is available. Think though how often you have thru lack of planning forgot to do something really important?
And I confess to being confused by the term drug seeking. Given that about 95% of all non-surgical visits end in a prescription, aren't all patients drug seeking. I have never heard anybody talking about Ventolin seeking or nitrate seeking or Amoxil seeking patients.
Which reminds me. I used to work in the ER and see the patients like the ones described in the rant. They were a pain in the butt, but they did pay the bills if you are on fee for service. Its a hell of lot easier to order Demerol and Gravol, or whatever your migraine cocktail is, than it is to actually figure out a sick patient. And, unless things have changed since I was an ER doctor, about half the doctors just order that to the regulars without even seeing them. Of course when I covered a ER without on-site coverage it was a pain to come in from home which is why most of us just left standing orders for the 10 or so ER regulars every small town had. I can however see why you are upset about having to treat these patients. You are of course very busy with other duties in the ER (which judging from the wrecks who come up to OR from the ER doesn't include working up or resuscitating surgical patients).
When I worked in the emergency room, it wasn't the "drug seeking" patients who bugged me. I actually enjoyed the mental chess games they played with me. What bugged me were the non-compliant patients with chronic diseases who showed up with their suitcases packed asking to be admitted, the patients who came with URTIs and of course the doctors who sent their patients to the emergency room expecting you to work them up and arrange the admission. Not to mention being yelled at by specialists when I wanted a consult.
And who gives a shzt that apparently all emergency room docs were in the top 25% of their medical school classes and are therefore harder to fool. Actually I think anybody who got into medical school is pretty smart. No that's wrong, anybody who got into medical school got good marks, did the appropriate volunteer work and was able to suppress their antisocial personality traits in their admission interviews. This is not the same as being smart. I graduated 44th in a class of 89 (not at the top of class but at the top of the bell curve) and I did okay. With much of medical school marks being passed on subjective rotation evaluations, the fact that you were in the top 25% just means that you were probably good at brown-nosing and back stabbing your fellow students to make them look less good and you look better. Those of us in the bottom 75% remember just what absolute zib-zabs most of the top 25% were.
And oh yes, 30 years ago when I started practice in Canada emergency rooms were staffed by what we called general practitioners on rotation duty plus a few full-time emergency room physicians who were either young doctors fresh out of their internship or older doctors who had given up their practices. And you know what? The care that patients got was just as good then as it is now. If anything it was little better because these individuals knew their limitations.
Just something I had to get off my chest.
Friday, September 20, 2013
My Skill Set No Longer Matches Your Needs
This is such a great statement that describes how I feel when the Pain Clinic patient shows up asking me to write a letter to fix their disability claim, their WCB case or any of the other jobs I do in the Pain Clinic which they never taught me about in medical school.
Now a lot of the patients I see in the Pain Clinic have been really fzcked over by the system and I used to be happy to spend hours on the phone, fill in forms or write letters I know nobody will read on their behalf. I am really amazed that patients think my opinion is that influential.
I know that most of the patients I see in the Pain Clinic are never going to go back to work but I do my best to try and make them more comfortable and functional. This is difficult sometimes when you spend most of the visit discussing how the patient can maximize their income support from various sources.I have become less tolerable of this complete waste of my time. I now have a stock response to the patient who complains about his treatment at the hands of Workers Comp:
You have 3 options:
1. You can do what they tell you to do.
2. You can hire a lawyer.
3. You can forget about your WCB claim and get on with your life.
For disability insurance problems, I usually advise them to get their union involved (in the small minority who have a union), or get their employer involved (he usually paid the premiums so might be interested). For welfare problems, I advise them to see their member of the legislature (it's amazing, then again maybe not, how few people know who their MLA is). One of the better funded pain clinics in our province actually has an "Entitlement Group" where patients can learn how to navigate the system.
There is of course the patient in whom I do write a letter who brings the letter back demanding revisions or asks for another letter because the letter I sent didn't get the response they were looking for. All this doesn't necessarily make me popular, like the other blogger says, "My Skill Set No Longer Matches Your Needs".
Gold Plated Equipment
We use a lot of advanced equipment in anaesthesia and a lot of what we use has become more complicated an expensive since I have been in practice.
On the other hand, consumer goods have become more complicated but less expensive over the same time. For example I paid $600 ($1259 in 2013 dollars) for a VCR in 1983. Assuming I could even find one, I suspect I would be paying about $50 now in 2013 dollars. I bought a Blue Ray player at Costco for $100 last year. My first desktop computer with 1 megabyte of RAM cost $4000 in 1991. My latest lap-top cost just over $400. What is most medical equipment except a big computer?
As the article points out, even allowing for a modest profit, it is possible to build a videolaryngoscope for a lot less than we currently pay for one. A couple of weeks ago while walking thru Costco, I found a flexible fibre-optic camera on sale there for about $100 complete with a videoscreen. This would be useful for plumbers but it could have all kinds on other uses, like looking for the stuff that falls behind my desk. Or as I told my wife, a home sigmoidoscope. This just shows how cheaply a fibreoptic device can be made nowadays.
I wonder how much of the healthcare costs which we are told are spiralling out of control are due to the capital costs of "medical grade" equipment that we have to buy. In a country like Canada which has for all intents and purposes no electrical manufacturing sector, this means a transfer of our tax dollars to places like South Korea and China not to mention the money that gets skimmed off by American or European middlemen we have to deal with. A country with a population of 30 million like Canada could probably produce it's own cheaper medical devices on a break even basis, paying workers good wages but that would require government intervention and even a bleeding heart liberal like me doesn't trust the government that much. Bulk purchasing has been shown to work although getting multiple hospitals and practitioners to agree on one product is next to near impossible plus you give one company a monopoly and the quality of service goes down.
One of the effects of high prices is that sometimes hospitals just won't buy a piece of equipment you feel is necessary because it is too expensive. This affects surgery less than anaesthesia and a lot of the equipment we feel we "need" adds nothing to patient care; however I remember the struggle to get pulse oximeters in the mid-late 1980s. They cost $10K then despite not being much more sophisticated than a VCR and it wasn't until the price came down and (less importantly) practice standards came out that their adoption became universal.
Now of course medical equipment is a little different from consumer equipment in that it has to be sterilizable and may have higher standards of electrical safety but certainly not enough to justify the huge mark-up which as the article points out is only equalled by crack cocaine. It would be great if for all that extra money went towards a more durable product but we all know how much downtime medical equipment spends being serviced and the cost of that service.
One of the plastic surgeons told me he was going to do video-assisted carpal tunnel releases in his office. Instead of the expensive monitor the company wanted him to buy, he just went to Best Buy and picked up a flat screen TV. Expensive monitors have proliferated all over the ORs and endoscopy suites which are probably no more sophisticated (maybe less sophisticated) then the brain-sucking Big Screen TV in my mancave but probably cost 10X as much.
Consumer health products do not seem to affected by the mark-ups that the hospitals pay. You can buy a home ECG monitor like this, or a finger pulse oximeter for under $100. Devices with cables that work with your i-phone are now available.
This remains one of the real scandals in medicine and it would be nice if our politicians and media stopped harping on how much doctors and nurses get paid and looked into this.
Friday, August 30, 2013
Non-therapeutic touch
This post is puts it more eloquently than I ever could and to our credit (and to everybody elses discredit) is written by an anaesthesiologist.
Right on. During the touchy-feelie parts of medical school I had to endure, they talked about the importance of touching patients and how to do it in an appropriate fashion. Aside from the touchy-feelie aspects, we learned in our physical exam sessions that you could actually get useful information like skin temperature, clamminess, edema and texture just by touching patients. I haven't come across it yet but I suspect some people are now donning gloves just examine patients or take their blood pressure.
Nobody likes to be a vector for infection but our infectious disease department expects you to wash your hands before AND after wearing gloves so the gloves are mainly for your aesthetic protection. I wear them now for starting IVs and doing injections in the Pain Clinic but I know they don't protect against needle-sticks.
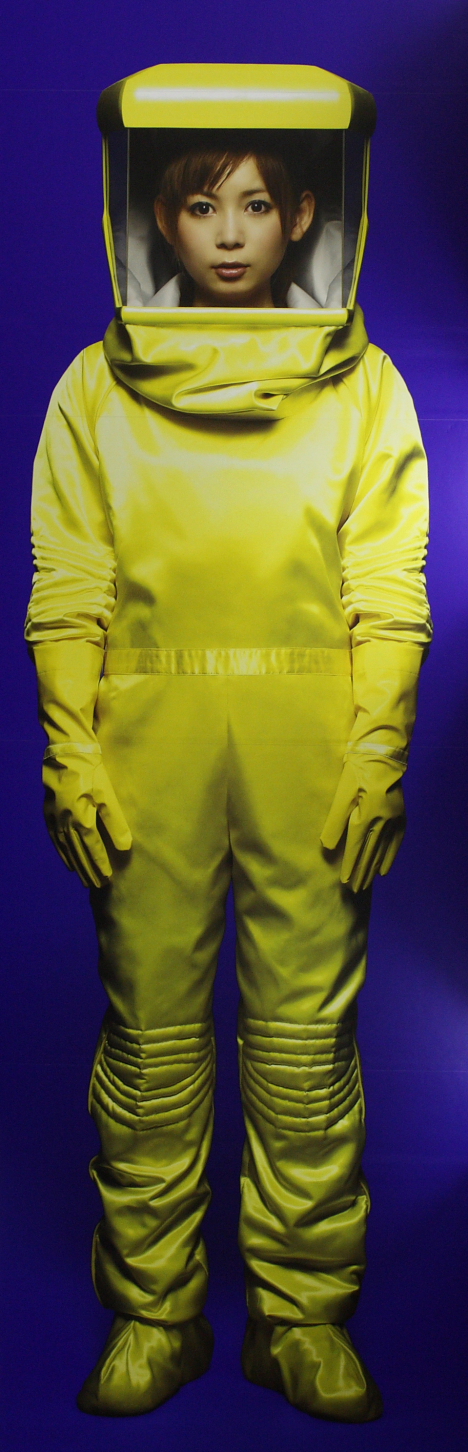
Patients in isolation are another matter and the odd time I have to assess a patient either as chronic pain consults or for anaesthetic purposes, I feel like my hands are metaphorically tied behind my back. Trying to assess and counsel a patient while dressed up in a yellow gown, paper hat, mask and gloves sends the wrong type of message to the patient at what may be a stressful time for him plus it makes the examiner so uncomfortable that I at least just want to get things finished and get out of there as quickly as I can. Hardly good medicine.
As the author points out there is a great deal of information that can be obtained with a good stethoscope and I must admit that in the holding area, I am often remiss in this. Stethoscopes according to our infection control department are difficult to sterilize without damaging the plastic. They haven't gone as far a banning stethoscopes which would really look bad, not that more than half of doctors even own one now, but are just ignoring this.
Laennec's stethoscope here is easily sterilized. Maybe we should go to this one.
Thursday, August 29, 2013
Crying wolf
I found this neat article on kevinmd (which despite having such a stupid name has some good stuff)
I still remember the first time I went into an operating room in second year medicine. The one thing I remember was the sepulchral quietness of the room, the sound of the ventilator bellows, the beep of the EKG monitor, the Muzak in the background and the hushed voices. If you went into any operating room today, it is a pretty good chance that at least one alarm will be going off.
I suspect that if most anaesthesiologists are like me, they spend a few minutes a day turning off as many alarms as their machine and monitors will allow. Because they are annoying and they distract you from the alarms and sounds you actually need to hear. (Actually one of my colleagues sets the alarm limits so that the alarms will go off all the time when he is working afterhours because they keep him awake.)
In 1986 when I started my residency there were very few monitors or alarms. We had an EKG, a manual blood pressure cuff and some people used a precordial or esophageal stethoscope. When we got the pulse oximeters many surgeons complained about the extra beep. (The ENT surgeons of course hated them because they showed how much patients desaturated during endoscopies). Now we have NIBPs which will alarm if the pressure is too low or high or more frequently because they can't get a reading, EKG with their alarms for high and low rates (the new monitors we bought had QT interval alarms which given that anaesthetics increase the QT, alarmed continuously until we figured out how to turn them off), ETCO2 and who knows what else.
Alarms on machines have proliferated. The first machines I used as a resident had disconnect alarms and oxygen monitors which alarmed if the FiO2 dropped below a limit. These were actually after-market devices which where added onto the basic machine which was sold with no alarms at all except for the ingenious fail-safe whistle which went on if the oxygen supply failed.
It was early in my residency that our local Centre of Excellence purchased it's first Drager machine not affectionately known as Herman. Herman had alarms for everything and gave an annoying de-da-de-da-dot over and over again. The Drager rep proudly told me that they had done research and had ascertained that this combination was the most annoying and difficult to annoy combination of sounds. Thanks guys. We are currently trialling machines at our hospital. I asked the rep if it was possible to customize alarms like cell phone ring tones. I suggested that I would like "Another One Bites the Dust". He laughed a little nervously.
Now every anaesthetic machine comes with an array of alarms for a variety of conditions. Some of them I don't even understand. There are alarms like High Inspired Gas which goes off when you are trying to do a mask induction and low MAC which goes off when you are trying to wake a patient up or doing TIVA with a little gas for your own piece of mind. When I get the alarm, I first look at the sat, the ETCO2 trace see if the patient seems to be getting anaesthetics and oxygen and then randomly make adjustments until the alarm turns itself off. To turn off or adjust the limits on many of these alarms it is necessary to hunt through multiple menus until you get to where you are at. This just distracts you from important things you could be doing like reading the paper, surfing the internet and oh yes monitoring the patient.
On top of this we have other alarms besides ours going off in the OR like the tourniquet which alarms after an OR plus on top of that we have the artificial noise from the cautery. The electrical beds our hospital recently bought emit a piercing alarm when the bed is unlocked (i.e. when you are moving a patient in or out of the OR on his bed).
We started doing endoscopy sedations about 2 years ago. After a few weeks, the supervisor came to me and asked if I could get my staff to either a) turn the alarms off or b) do something about them. The major culprit was the ETCO2 alarm attached to the nasal prongs. As I found out a few months ago when I tried using it, no matter how you set the limits it basically continuously alarms even in conscious patients whom you haven't even touched yet. Despite this our national association has made this a standard of care. I suspect the wise people who make these standards are academic anaesthesiologists who haven't given a real anaesthetic without a bevy of techs and residents to hold their hand and wipe their bum in years. Some people have advocated that the people we currently monitor on the ward with pulse oximeters should get these ETCO2 monitors instead. I can only imagine the frustration of the nurses at the false alarms generated by these machines and speculate at how long before one gets pitched thru the window.
And of course it is when the shit is actually hitting the fan that the alarms become most annoying. Like, yes I know the BP is 40/0 and I am trying to do something about it so shut the fuck up! Our recovery room nurses are forbidden to turn off or silence alarms so the odd time I bring a patient out with sats in the 80s I have to listen to the alarm until oxygen is applied and the sat comes up on its own as it mostly always does.
It would be nice if we could say that most of the alarms actually enhance patient safety. Anaesthesia is a lot safer now than when I started in 1986 and not because we have more alarms but because we have the pulse oximeter. And further it is not the cut-off point of the alarm which is important. A gradual drop in the SaO2 from 99 to 94 probably needs to be looked at and if you are going to wait for the alarm to go off at 90 you may have missed the boat. Curiously most of our pulse oximeters have a default setting of no volume on the pleth so I have to actually turn this feature on every time. Likewise a gradual trend upwards in the heart rate may indicate something sinister well before the high heart rate alarm goes off.
I am certainly not advocating returning to the state of monitoring which existed when I started my residency. I remember as an intern working with the Professor of Anaesthesia who lectured me over the whole day on how much monitoring was unnecessary and how he hardly ever put EKG electrodes on his patients (he even knew how much each one cost). It would of course be interesting to know how much we spend on EKG electrodes per event recognized and treated and I suspect it is thousands of dollars, not that I am going to give up my EKG.
Tuesday, July 23, 2013
Something I could have written myself albeit less eloquently
Friday, July 19, 2013
Oh Professor
I digress.
I have never been the outstanding academic student. Like many doctors I was usually near the top of my class in grade school, rarely at the top. Conventional wisdom when I was an undergrad was that you needed an 85% average to get into medical school, that is exactly what I got no more, no less and I got into medical school. I don't think I am terribly smart, I do and have done a lot of stupid things. It is just that it is almost like the school and university system was designed for me to excel without really trying that hard.
Entering medical school, it occurred to me that I could become an outstanding academic doctor or I could just scrape through. Within the first few weeks of medical school it became quite apparent that a significant number of my classmates were either, smarter than me, prepared to work a lot harder than I was, or smarter than me and prepared to work a lot harder than me. With that in mind, I focused on first passing and secondly learning the minimum I would need to become a good doctor. Some things interested me more than others and I paid more attention to those. I tried to have as normal a life and as much fun as possible and more or less succeeded. I sat in the back of the lecture hall, read the newspaper if the lecture was boring and made fun of the keeners who sat at the front and asked questions. I also drank mass quantities of beer on Friday and Saturday nights and not infrequently on weeknights.
I treated internship like a job and did very little reading, I figured if I hadn't graduated with the basic knowledge, something was wrong. Sailing was more or less smooth. One night when I was woken up to do an EKG on an ICU patient (ICU nurses can't do EKGs go figure), one of the nurses told me, "at least next year when you are a resident you won't have to do this." I told her I had no intention of ever being a resident.
Specialties never interested me. When you are 24, the idea of spending what amounts to 1/6 of what you have already lived in servitude was less than attractive.
For various reasons I only lasted 3 years as a general practitioner. Deciding to go back into a specialty was for me a huge life change, which I didn't undertake lightly without considering other career options like law school. I remember the feeling of "what the hell have I signed up for" on my first day. Fortunately I took to anaesthesia like it was like I was born to do it. I was a little scared about the whole academic aspect of it so I read from day one (actually I bought the textbooks before my residency) as opposed to the residents who weren't scared of the whole academic aspect who didn't feel pressured to read. I had never enjoyed giving presentations but now I had to give them so because I was so scared of being publicly humiliated (which was legal to do to residents them) I actually worked hard on them and came up with some incredibly polished presentations amazing myself.
I was surviving even thriving in academia but I knew it wasn't for me and after finishing my residency my first job was in a community hospital. About 1 and a half years into what I still remember fondly as a pleasant sojourn as a community anaesthesiologist, for reasons I still can't figure out, I answered an ad to work at the Centre of Excellence.
In a perfect world academic teaching hospitals would go out of their way to attract the best and brightest clinicians financially and otherwise. In reality, unless you have gotten onto the Geographic Full Time (GFT) gravy train or have a subspecialty interest which your academic centre supports, they are soul-destroying factories where one puts in time while waiting for a position at another hospital in town to open up. Positions at other hospitals were not forthcoming in the early 1990s; later when jobs were more forthcoming a lot of the bright minds brought to the Centre of Excellence did not even pretend to be interested in working there for the long term and actively sought work elsewhere within months of arriving. Jobs at other hospitals as I mentioned were not available when I arrived at the Centre of Excellence; I settled in and when the opportunity to run the Pain Clinic came up I took it which made me a sub-specialist.
With my appointment at the Centre of Excellence came an academic title. This initially was Clinical Lecturer although the chairman assured me that I would soon be elevated to Clinical Assistant Professor. The title came with no money attached and no real perks beyond a library card, the ability to use the University's gym for a discount and the ability to join the Faculty Club for the usual fees. There is however a certain cachet to an academic title although maybe I am the only person who thinks that way. I am a little reminded of the episode of Cheers where Rebecca gives Sam and Woody titles instead of a raise.
My academic career remained stalled at Clinical Lecturer for about 7 years, (I am sure the chairman just forgot) but I was eventually "promoted" to Clinical Assistant Professor and then Clinical Associate Professor.
Running the Pain Clinic made me the expert on chronic pain in a University Teaching Hospital which lead to requests to give talks and to lecture the medical school which I took on. I even got invited to speak at national meetings and eventually developed a pretty impressive academic CV. I was a little evangelical and ambitious with respect to chronic pain; I always looked on talks as a way to solidify my standing and build my referral base.
After 13 years I finally left the Centre of Excellence. I noticed soon after I had been dropped from list of part-time academic staff on the University Department's website, so I figured I was no long a Clinical Associate Professor and took if off my CV and letters. After about 3 years, I did get a letter from the Dean re-appointing me. About a year ago in the spirit of "glasnost" the new Chairman invited staff at community hospitals with University appointments to apply for promotions, so I thought what the hell and applied. A few months later the assistant Dean, who I play saxophone with, congratulated me. "On what?", I said. "Your promotion," said the assistant Dean and that was how I knew that I was now a Clinical Professor.
The University made up a nice plaque commemorating my new exalted status and the Chairman presented it to me last week over dinner which the Department paid for. Periodically somebody I haven't seen for a while runs into me and congratulates me. "For what?" I say and they say, "For your professorship", so I guess it is a really important thing, even though I tell people a Clinical Professorship and $1.65 will buy me a coffee.
Somebody at a talk I attended pointed out that most doctors are a little insecure and believe that they are frauds and are just waiting to be found. I knew right away he had me down and I am still waiting for somebody to come and tell me I am full of bullshit and puncture my balloon. I still think of myself reading the sports section in the back of the lecture hall and my general distaste for academia. In some ways I feel a little sheepish, in others I am thumbing my nose at every academic doctor who talked down to me. Because hey, I am a Full Professor now and money can't buy that title.
Sunday, July 7, 2013
Work-life balance
Opioids, a personal journey
I found this article on Kevin MD
20 or so years ago I started treating chronic pain in a University Pain Clinic. Actually it was just me and the Day Ward nurse who drew the short straw in a corner of the Day Ward that nobody else wanted to use but we called it a pain clinic. I like to bore people by telling them how we used to treat patients with chronic pain in those days. I basically had 3 tools: needles, amitryptiline and carbamazepine.
Needles actually worked in more patients than should have been scientifically possible but didn't work in everybody. Amitryptiline and carbamazepine work well in randomized double blind trials and in meta-analyses but work poorly in the real world I started exploring other anti-depressants and anti-convulsants. A patient brought me the article on the first case series of 9 patients treated with gabapentin and I still look on that moment as a milestone in chronic pain management. Gabapentin also only worked in a small fraction of patients.
I started sending patients to the hospital psychologist who, when she realized what was going on, rationed me to one patient a month; the physiotherapy department refused to see chronic pain patients. Don't worry, I was told any time now we are going to get a big multidisciplinary pain clinic. Fortunately I didn't hold my breath on that one.
Quite a few of the patients that came to the pain clinic were taking fairly substantial doses of narcotics. In fact that was the primary reason for referral for most of them. This was usually tylenol with 30 or 60 mg of codeine or tylenol with oxycodone. There were the other standbys, talwin, darvin and fiorinal and quite a few patients were on injectable meperidine either thru their doctors office, the emergency department or some actually self-injected.
At this point I should back-track to what I knew about narcotics in chronic pain which was not very much. I believe we had one lecture in medical school in first year. This lecture was by someone from the College of Pharmacists talking about prescription drug abuse. I don't remember many lectures in medical school; I remember this one vividly if only because it was the first and last time I heard patients referred publicly as assholes. Other than pharmacology we didn't get much teaching on how to order narcotics either in acute or chronic pain. The use of narcotics in palliative care was only just starting. During my first surgical rotation, the surgery resident told me how to write the post-op orders which consisted mostly of: "Demerol 75-100 mg IM q3h PRN." (I would like to think this has improved except I don't think is has, except that Demerol is hard to come by.)
When I started in general practice and covering the emergency it became apparent that a lot of patients had chronic pain. Except we didn't call them chronic pain patients then, we called them addicts and drug seekers. In the emergency quite a few docs didn't even bother seeing them. "Oh so and so is here again," they would say as they wrote an order for the nurse to give 100 mg of Demerol. Some GPs just phoned it in or left a standing order so they wouldn't have to come in from home in smaller hospitals where there wasn't on site coverage. I remember in my first locums being alarmed at just how much narcotics and sedatives people were being prescribed. Nobody told me about that in medical school. To be sure, a lot of them were abusing their drugs. There were stories about doctors being threatened by patients for not prescribing what they wanted. I was never threatened but a friend of mine was by somebody just passing through town when my friend wouldn't prescribe the patient's choice of oral narcotic. A lot of them however especially when you got to know them had legitimate pain problems, they had had multiple back surgeries or suffered from intractable migraines and while there was a lot of tut-tutting about their narcotic use, there wasn't a lot of effort being made to see if they could be helped in another way.
There were a lot of valid reasons why I fled general practice (like not being very good at it) but I have to think that seeing those patients day after day and night after night and knowing I really had nothing to offer them that pushed me just a little bit.
So it was that 7 or so years removed from general practice my opinion of narcotics in chronic pain both from training and experience was pretty dim. They were never appropriate and patients who used them inevitably became addicted which was a bad thing even if they did seem to help some people's pain.
The tide was changing. Use of narcotics in palliative care had become accepted, it was noted that patients could tolerate high doses with reasonable function and long acting oral forms were available freeing patients from injections. Because nobody wanted to see chronic pain patients, a lot of palliative care physicians reluctantly saw these patients and used what they were familiar with which was long acting oral narcotics And some patients actually got helped. Around 1993 our provincial college (Medical Board) actually published guidelines on the use of narcotics in chronic pain.
In 1995 at the Canadian Pain Society Meeting, I first saw OxyContin advertised. My experience with patients who were taking oxycodone/acetaminophen preparations in Canada, lead me to believe that the oxycodone molecule had some special properties that other opioids didn't have. I remember telling the rep manning the booth that OxyContin was going to be huge drug. Occasionally I am right about things.
I don't remember when I wrote my first long acting narcotic script. It should have been a memorable experience but it wasn't. I do know that it took two years for my to write my first 50 triplicate prescriptions and I was seeing a lot of patients in that era. What I do remember is that when I wrote these prescriptions for people who had failed needles, amitryptiline, carbamazepine and even gabapentin, a significant number of patients actually seemed to improve. It was actually fun seeing them for their follow-up visits because they were actually happy. This wasn't everybody of course and many people who aren't satisfied with their treatment just don't show up for follow up visits. (I always assumed they didn't show up because they were better but of course I know that usually isn't true.) I got a methadone licence and started prescribing methadone with great gusto as well.
I started even feeling dirty when I did a block on somebody instead of whipping out my triplicate pad.
I started seeing people at meetings talking about their experiences treating chronic pain with opioids. What I noticed was that they presented the same small group of cases again and again as if this was maybe their only success. It didn't matter, I drank their Kool-aide; after all we had very little left to treat the majority of our chronic pain patients. Pretty soon I got approached to start doing those talks locally. I was still evangelical about pain and to Big Pharma's credit, I was never told what to say and while they provided slide kits, they never minded.when I modified their slides when I didn't agree with what the content.
The gospel my fellow travelers and I preached was:
- You cannot be addicted to your pain meds if they are prescribed for legitimate pain.
- There is no maximum dose of opioids.
- Opioids are safe and there is no end-organ damage.
- Opioids are efficacious in chronic pain.
- Controlled release opioids are preferable to short-acting opioids.
You cannot be addicted to your pain meds if they are prescribed for legitimate pain.
Opioid hyperalgesia was something our palliative care colleagues had observed for some time and I still see this in many patients I see, usually other people's patients but sadly a few of my own. It is hard to tell them that the answer to their pain is less rather than more opioid. Strangely many of my colleagues continue to disbelieve that this exists; some of them get out right hostile if you discuss it.
Opioids are safe and there is no end-organ damage.
Published guidelines supported (mandated) the use of controlled release opioids so if you prescribed short acting opioids because that was what seemed to work, you could face discipline.
Controlled release opioids were, of course, more expensive and less likely to be generic.
And so a new era in pain management began
With all this in mind my fellow pain specialists and I began prescribing with great gusto. Many family docs who attended our talks also took this up. Many of course steadfastly refused to have anything to do with what was supposed to be the future of pain management. We knew they would eventually come around. I acquired more colleagues who had done pain fellowships in the US and were versed in the gospel of oral narcotics. They were for the most part against interventions so I began to feel guilty when I did a procedure. Besides it was so much easier to whip out the old triplicate pad.
Even the local entrepreneurial physiatrist with the "multi-disciplinary" pain clinicwho had previously preached against opioids got in on the act. He realized that it was much more cost-effective to prescribe methadone than to have to pay for physiotherapists and psychologists.
It became common to see patients on very large doses of OxyContin or another narcotic, usually with another short-acting agent for breakthrough, sometime two long acting opioids.
And then of course the shit hit the fan
Now it is not like there was no prescription drug abuse before OxyContin. During my time in general practice we knew patients abused codeine products, dihyrocodone(DH) cough syrups, and Talwin among others. Even during the worst of the OxyContin "epidemic" of drug abuse, Tylenol with Codeine was as popular on the street as was OxyContin. OxyContin was different from other pills in that much higher doses of narcotic were packed into each pill, as much as 80 mg. And then there was the supply.
Being a sub-specialist I never was exposed to how OxyContin was marketed at the primary care level. I did however give a lot of talks to primary care, where without mentioning OxyContin specifically, I outlined the five points above on how appropriate, safe and efficacious it was to prescribe long acting opioids for chronic pain. And OxyContin was a very effective well tolerated narcotic which meant that it became the go to drug for family docs which meant that there was a lot of OxyContin around to leak onto the streets.
Pretty soon we heard about "hillbilly heroin", lives ruined through OxyContin and people dying of overdoses. I have always wondered who is at fault when somebody lies to their doctor, buys or steals a drug to get high. Is it the drug or it is the person? I am sort of leaning towards the person. I would see parents on TV talking about how their son's or daughter's life was ruined through OxyContin as if maybe the way they were raised didn't maybe have a little to do with it?
Nonetheless licencing bodies and governments clamped down. Family docs read the stories and didn't want to prescribe OxyContin or for that matter any narcotic. Pharmacies wouldn't carry them. Patients refused to take them.
In Canada a mulidisciplinary group on opioid use published a document stating that 100 mg of oral Morphine was the "watchful" dose which means that that was the dose at which you were supposed to re-evaluate things but of course licensing bodies and insurance companies interpreted this as the maximum dose.
Companies responded by trying to make their drugs more tamper-proof or by adding naloxone to foil IV drug use. This is partially helping. I am told that since CR Oxycodone is now tamper-resistant, illicit oxycodone use has gone down, replaced (surprise, surprise) by heroin use.
So did we (I) learn anything from this?
I like to think so. I screen for addiction a lot more now and I like to believe I am more cautious. I don't push the dose, I figure if they aren't getting relief at lower doses, it may be time to look at another medication or another therapy. I'm not ashamed to do blocks if I figure they might work. The bottom line is, I still prescribe oral opioids including controlled release Oxycodone.
A lot of doctors have however been scared off from prescribing narcotics in any form. On top of this, because there is now a shortage of family docs, many family docs will not see any patient taking opioids, quite a few won't see any chronic pain patient just in case. This of course puts more pressure on those of us doing chronic pain management and we all know that if we, after exhausting all options, trial the patient on oral opioids, we have more or less married them.
A few "experts" are also piling on stating that narcotics will inevitably lead to addiction (which given the rigid definition they use is an almost certainty). I actually read somebody who wrote that palliative patients shouldn't be prescribed opioids.
Some of my fellow co-disciples from the old days don't seem to have learned. I get some hostility at meetings when I suggest that the ways we practised and encouraged others to practise may not be appropriate anymore and we should maybe be a little judicious about prescribing opioids.
One of the advantages of getting old is of course seeing how heresy becomes dogma and dogma becomes heresy. And of course oral opioids are just another medication fad that didn't work out as well as it should have. For example:
Sunday, May 19, 2013
NPO
Anyway one of these urgent stones presented to the OR in the evening having just eaten a full meal. I didn't find out why this happened but I suspect the patient thought he was coming to the hospital to consult with the surgeon about his stone, NOT to have surgery. It could have been that he got faulty instructions from the surgeon's office or that he is just stupid but he admitted to having eaten supper. "That is too bad," said my colleague, "I guess you will have to have your surgery tomorrow." "But" replied the surgeon, "he needs to have the stone done or else he might get septic!" "Fine," says my colleague, "After a solid meal he will need to fast for 6 hours." "That is way too late," said the surgeon, "he is going to get septic, can we do him under local with IV sedation." "You can do what you want," replied my colleague, "But you are on your own" and went off to cool his heels. The surgeon according to seemed shocked.
Kidney stones do get septic, I have seen one case in my medical career but as even the urologist who is chief of surgery at our hospital acknowledged, this is rare. I suspect the urologist in this case was more concerned about getting home to tuck in his kids and have sex with his wife than any impending sepsis.
It does bring up the interesting topic of NPO.
When I started my residency a 6-8 hour fast usually written as NPO after midnight was the rule which meant patients frequently fasted for 16 hours or more. The 6-8 hour fast was not based on any real evidence. Up until the late 1950s fasting guidelines were much more liberal including things like tea and beef broth right up until surgery. The introduction of longer fasting intervals coincided with other things like better anaesthetics (like halothane instead of ether), more use of endotracheal intubation, better trained anaesthesiologists and intensive care units, so any attribution of decreased morbidity with aspiration is more multifactorial rather than just due to longer fasts. There also emerged a dogma of a gold standard of a gastric volume of less than 0.4 cc per kg and a pH of greater than 4 based on research on Rhesus monkeys extrapolated to humans.
Further we were told that narcotics delayed gastric emptying as did a myriad of other medical conditions including pregnancy so that those patients all had to have their airways protected with a rapid sequence induction and an endotracheal tube. We asked every patient about reflux.
Many patients of course needed their surgery immediately and we managed them with rapid sequence inductions. It was also apparent that one could use the NPO interval to manipulate emergency cases. If you thought you could get the case put off to the next day, you quoted a longer fasting time, if you knew you were going to have the do the case anyway, you accepted a shorter fasting time. I played that game fairly recently. Surgeons also clued in. When I was a resident, I was on call and one of the older surgeons booked an appendectomy. "He ate lunch," said the surgeon smirking, "So how about we do him at 7 pm?". What this really meant was he wanted to go home and have supper and then come back to do his case. I on the other hand was more interested in following the list with the case. As I told the staff anaes firstly the patient had to be treated as a full stomach anyway and secondly if he was actually able to eat lunch, they didn't have appendicitis. It didn't work, staff surgeon and anesthesiologist ate supper at home, I ate supper in the hospital cafeteria after which the patient was relieved of his appendix.
Already as I started my residency, brave anaesthesiologists were actually doing research to challenge the dogma of NPO after midnight. One of them who gave a talk at rounds described how some of his fellow anaesthesiologists were horrified and refused to even be in the room while he did the studies. It became clear however that patients could actually have clear fluids right up to the time of surgery and now the Canadian Anesthesiologists Society recommends allowing clear fluids up to 2 hours pre-op. Administration asked about 3 years ago if we would relax our NPO standards at our hospital, I looked at the guidelines, asked my colleagues and we agreed that people could have water up until 4 hours pre-op just in case the case before them was cancelled. We chose water because of the confusion over what exactly is a clear fluid. The hospital ignored us and rolled out a 4 hour clear fluids policy with huge fanfare this January, however most patients seem to be fasting after midnight.
Exactly what a clear fluid is, has never been clarified. If you look at the variety of fluids that are considered to be clear fluids, you see a variety of fluids with different pH and often pharmacological properties on their own (tea or coffee). Many patients think that a large milkshake is a clear fluid. I suggested just telling patients to drink Gatorade (any colour except red) which is what my surgeon told me I could drink before my colonoscopy. I am not endorsing Gatorade, it could be Poweraid, Kool Aid or Tang. Coffee was verboten until they found it actually raised gastric pH and lowered gastric volume so black coffee is now back in. I still am not sure what adding a few mls of milk or cream does to make coffee any less safe.
A few years ago, one of colleagues at the C of E announced that she had just cancelled a patient for chewing gum. "Whats wrong with gum?'" I asked (as long as they spit it out). She looked at me like I was an idiot. "Gum increases gastric volume," she said the voice one uses when trying to explain something to a child. A few months later a study showed this wasn't the case. I should have copied it and put it in her box but I didn't.